Red blood cell antibodies play a crucial role in the body’s immune response, particularly in relation to blood transfusions and pregnancy. These antibodies are proteins produced by the immune system in response to the presence of foreign red blood cells. When we receive blood from a donor, the immune system checks for compatibility. If incompatible blood is introduced, the body may produce antibodies against the donor’s red blood cells.
This reaction can lead to serious health issues, making it essential to understand and identify antibodies through precise tests. The presence of these antibodies can significantly impact health, especially for individuals requiring frequent blood transfusions or pregnant women with potential blood type incompatibilities.
Key Takeaways
- Red blood cell antibodies are proteins produced in response to foreign red blood cells.
- These antibodies can cause serious health issues in cases of incompatible blood transfusions.
- Pregnant women with blood type incompatibilities are also at risk due to red blood cell antibodies.
- Precise tests are crucial for identifying and managing these antibodies.
- Understanding red blood cell antibodies is vital for healthcare professionals and patients alike.
Understanding Red Blood Cell Antibodies
The formation of red blood cell antibodies is a complex process involving the immune system’s recognition of foreign antigens. Your immune system is designed to protect you against harmful invaders, and it does so by producing antibodies against substances it identifies as foreign.
Definition and Basic Function
Red blood cell antibodies are specialized proteins produced by the immune system that recognize and bind to specific antigens present on red blood cells. These antibodies serve as the body’s defense mechanism against foreign red blood cells, which may enter the bloodstream through transfusions or during pregnancy. Understanding the basic function of these antibodies is crucial for preventing adverse reactions during blood transfusions and managing potential complications during pregnancy.
How Red Blood Cell Antibodies Form
The formation of red blood cell antibodies typically occurs when an individual is exposed to red blood cell antigens that differ from their own. This exposure can happen through blood transfusions or during pregnancy when the mother’s immune system may react to the fetus’s red blood cells if they carry different antigens. The process involves complex immune system responses, including recognition of foreign antigens, B-cell activation, and subsequent antibody production. Once formed, these antibodies remain in the bloodstream and can react with matching antigens if encountered again, potentially causing hemolytic reactions.
Types of Red Blood Cell Antibodies
There are several distinct types of red blood cell antibodies, each with different origins and clinical implications. Understanding these differences is crucial for proper blood compatibility testing and preventing transfusion reactions.
Naturally Occurring Antibodies
Naturally occurring antibodies, such as anti-A and anti-B antibodies, develop without prior exposure to foreign red blood cells. These antibodies are present in individuals lacking the corresponding antigen on their red blood cells. For instance, a person with Type A blood has anti-B antibodies in their plasma.
Immune Antibodies
Immune antibodies, in contrast, develop only after exposure to foreign red blood cell antigens through transfusion or pregnancy. These antibodies are a result of the immune system’s response to incompatible blood types. For example, an Rh-negative individual may develop anti-D antibodies after exposure to Rh-positive blood.
Rh Antibodies and Their Significance
Rh antibodies, particularly anti-D antibodies, are clinically significant immune antibodies that can cause severe hemolytic reactions. The Rh factor is especially important during pregnancy, as Rh-negative mothers carrying Rh-positive fetuses may develop antibodies that can affect current or future pregnancies.
| Antibody Type | Origin | Clinical Significance |
|---|---|---|
| Naturally Occurring | Present without prior exposure | Causes ABO incompatibility reactions |
| Immune | Develops after exposure to foreign RBCs | Causes hemolytic reactions, especially in transfusion or pregnancy |
| Rh Antibodies | Develops in Rh-negative individuals exposed to Rh-positive blood | Can cause severe hemolytic disease of the newborn |
What Are Red Blood Cell Antibodies and Their Detection Methods
We use various detection methods to identify red blood cell antibodies, which is essential for providing compatible blood for transfusions. Red blood cell antibodies are proteins that can react with specific antigens on the surface of red blood cells. The detection of these antibodies is crucial for ensuring safe blood transfusions and managing pregnancy-related blood incompatibilities.
RBC Antibody Screen
The RBC antibody screen is a primary laboratory test used to detect the presence of unexpected antibodies in a patient’s serum. This screening test is routinely performed before blood transfusions and during prenatal care to identify potential incompatibilities. The RBC antibody screen looks for circulating antibodies in the blood directed against red blood cells.
- The test involves incubating patient serum with reagent red cells containing known antigens.
- Observing for agglutination or hemolysis indicates the presence of antibodies.
- If the RBC antibody screen is positive, further investigation is required to determine the specific antibody present.
Direct Antiglobulin Test (DAT)
The Direct Antiglobulin Test (DAT) detects antibodies already bound to red blood cells. This test is important for diagnosing autoimmune hemolytic anemia and investigating transfusion reactions. The DAT involves using anti-human globulin to detect antibodies or complement proteins attached to the patient’s red blood cells.
Indirect Antiglobulin Test (IAT)
The Indirect Antiglobulin Test (IAT) identifies antibodies circulating in the serum that can potentially react with donor red blood cells. This test is crucial for selecting compatible blood for transfusion. The IAT involves incubating patient serum with reagent red cells and then using anti-human globulin to detect any antibodies that have bound to the red cells.
red blood
Understanding these detection methods helps healthcare providers select compatible blood for transfusion and manage potential complications in pregnant women. Positive test results require further investigation through antibody identification panels to determine the specific antibody present.
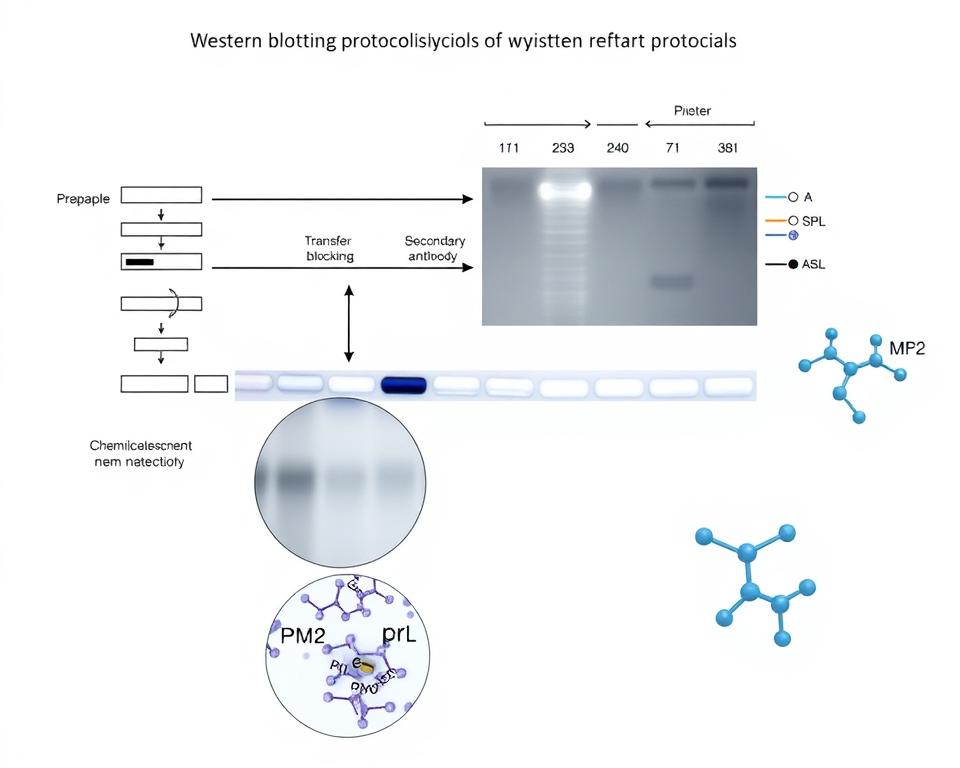
Western Blot Technique for Antibody Identification
We utilize the Western Blot technique to detect and identify specific red blood cell antibodies in complex biological samples. This sophisticated laboratory method operates on three fundamental principles: separation of proteins by size using gel electrophoresis, transfer of these proteins to a membrane, and detection using specific antibodies.
Principles of Western Blot
The Western Blot technique is based on the principle of separating proteins according to their molecular weight using gel electrophoresis. This process allows for the identification of specific proteins, including red blood cell antibodies, from a complex mixture of proteins extracted from cells.
Step-by-Step Western Blot Process
The Western Blot process involves several key steps: sample preparation, gel electrophoresis, electroblotting, and detection. During sample preparation, proteins are extracted from cells or tissues and denatured to break their complex structures. Gel electrophoresis separates the proteins based on their molecular weight, creating distinct bands for different proteins.
Advantages and Limitations
The Western Blot technique offers several advantages, including high specificity and the ability to detect very small amounts of protein. However, it also has limitations, such as being time-consuming and semi-quantitative rather than fully quantitative. Despite these limitations, the Western Blot remains a valuable tool for confirming the presence of specific red blood cell antibodies in complex samples.
Key Benefits: High specificity, ability to detect small amounts of protein
Limitations: Time-consuming, semi-quantitative
Red Blood Cell Antibodies in Blood Transfusions
Understanding red blood cell antibodies is essential for ensuring safe and effective blood transfusions. When a patient requires a blood transfusion, compatibility between the donor’s red blood cells and the recipient’s immune system is crucial.
Compatibility Testing Before Transfusion
Before a blood transfusion, we conduct thorough compatibility testing to prevent potentially life-threatening reactions caused by red blood cell antibodies. This involves:
- Blood typing to determine the patient’s blood group
- Antibody screening to identify any existing antibodies that could react with donor blood
- Crossmatching, where the recipient’s serum is mixed with donor red blood cells to detect potential incompatibilities
Transfusion Reactions Due to Antibodies
Transfusion reactions due to red blood cell antibodies can range from mild fever and chills to severe hemolytic reactions that can be life-threatening. These reactions occur when the recipient’s antibodies attack antigens on the donor’s red blood cells, causing hemolysis (destruction of red blood cells).
Prevention of Transfusion Reactions
To prevent transfusion reactions, we employ several strategies, including thorough pre-transfusion testing, selecting appropriately matched donor blood, and maintaining detailed transfusion history records. For patients with multiple antibodies, finding compatible donor blood becomes increasingly challenging and may require specialized blood bank resources.
Red Blood Cell Antibodies During Pregnancy
Red blood cell antibodies are a critical consideration during pregnancy due to their potential impact on fetal health. When a mother has RBC antibodies, they can cross the placenta and affect the red blood cells of the fetus, potentially leading to serious health complications.
Hemolytic Disease of the Newborn
Hemolytic Disease of the Newborn (HDN) occurs when maternal antibodies attack the red blood cells of the fetus, which can lead to fetal anemia, hydrops fetalis, or even fetal death in severe cases. The condition arises when the mother’s immune system reacts to antigens on the fetus’s red blood cells inherited from the father.
Rh Incompatibility in Pregnancy
Rh incompatibility is a common cause of HDN, happening when an Rh-negative mother carries an Rh-positive fetus. If the mother’s blood comes into contact with the fetus’s Rh-positive red blood cells, she may develop Rh antibodies. While the first pregnancy is usually not affected, subsequent pregnancies with Rh-positive fetuses may be at risk.
Prevention and Management
Prevention of Rh sensitization involves administering Rh immunoglobulin (RhIg) to Rh-negative mothers during and after pregnancy. Management of affected pregnancies includes monitoring antibody levels and assessing fetal well-being through ultrasound. In severe cases, intrauterine blood transfusions may be necessary.
| Condition | Cause | Effect on Fetus |
|---|---|---|
| Hemolytic Disease of the Newborn | Maternal antibodies against fetal RBCs | Fetal anemia, hydrops fetalis, or fetal death |
| Rh Incompatibility | Rh-negative mother, Rh-positive fetus | Potential for HDN in subsequent pregnancies |
Understanding and managing red blood cell antibodies during pregnancy is crucial for preventing complications and ensuring the health of both the mother and the baby.
Clinical Significance and Health Implications
The clinical significance of red blood cell antibodies is multifaceted, impacting transfusion medicine, pregnancy, and various autoimmune disorders. We will explore the implications of these antibodies in the context of autoimmune hemolytic anemia and their long-term management.
Autoimmune Hemolytic Anemia
Autoimmune Hemolytic Anemia (AIHA) occurs when the immune system produces antibodies against its own red blood cells, leading to their premature destruction and anemia. This condition can be primary or secondary to underlying diseases such as lupus or lymphoma. Diagnosis involves detecting antibodies bound to red blood cells using the Direct Antiglobulin Test (DAT). Treatment approaches include corticosteroids, immunosuppressants, and in severe cases, splenectomy or rituximab therapy.
Long-term Management of RBC Antibodies
Long-term management of patients with RBC antibodies requires careful documentation and communication between healthcare providers. Once formed, these antibodies persist indefinitely, although they may become undetectable over time. Patients with a history of RBC antibodies need special consideration during future transfusions to prevent hemolytic reactions. Health care providers must maintain detailed records of patients’ antibody profiles to ensure appropriate blood selection for transfusions.
| Condition | Diagnosis | Treatment |
|---|---|---|
| Autoimmune Hemolytic Anemia (AIHA) | Direct Antiglobulin Test (DAT) | Corticosteroids, Immunosuppressants, Splenectomy, Rituximab |
| RBC Antibodies | Antibody Screening | Careful Blood Selection, Monitoring |
Conclusion
The complex nature of red blood cell antibodies necessitates a comprehensive understanding for effective patient management. Throughout this article, we’ve explored the various types of antibodies and their detection methods, including the Western Blot technique. These antibodies play a significant role in blood compatibility, transfusion safety, and pregnancy outcomes. Healthcare providers must maintain accurate records of patients’ antibody profiles to ensure appropriate care over time. By understanding red blood cells and their interactions with antibodies, we can improve patient outcomes and prevent potential problems.
References and further readings:
1.Koul, S., Dahiya, P., & Pandey, S. (2025). Warm Autoimmune Hemolytic Anemia Triggered by Influenza A Infection: A Case Report. Authorea.
https://www.authorea.com/doi/pdf/10.22541/au.174921316.688341022.Rastogi, V., Sidhar, M., Rajesh, H., Kaushal, N., & Bhardwaj, S. (2025). Exploring Trends of Red Blood Cell Alloimmunization Among Transfusion Recipients and Healthy Blood Donors: A Comprehensive Analysis. ResearchGate.
https://www.researchgate.net/publication/3928705623.Jagnarine, S., Qiu, A., Kyritsis, E., & Dei Zotti, F. (2025). IgG2b Enhances Alloantibodies to Stored Red Blood Cells. Transfusion, Wiley.
https://onlinelibrary.wiley.com/doi/abs/10.1111/trf.183064.Wei, H., Chen, J., Ren, D., Zhao, J., Zheng, Y., Mu, S., & Yang, L. (2025). Novel Strategy for Overcoming Anti-CD47 Agents’ Interference in Pre-Transfusion Testing. Pathology, Elsevier.
https://www.sciencedirect.com/science/article/pii/S0031302525001849
FAQ
What is the role of RBC antibodies in transfusion medicine?
RBC antibodies play a crucial role in transfusion medicine as they can cause hemolysis or destruction of transfused red blood cells. We ensure compatibility testing before transfusion to prevent adverse reactions.
How do RBC antibodies form in the body?
RBC antibodies can form through exposure to non-self antigens during pregnancy, transfusion, or transplantation. We identify the type and specificity of these antibodies to provide compatible blood components.
What is the significance of Rh antibodies during pregnancy?
Rh antibodies can cause hemolytic disease of the newborn if an Rh-negative mother carries an Rh-positive fetus. We provide guidance on prevention and management strategies to minimize risks.
How are RBC antibodies detected and identified?
We use various tests, including the RBC antibody screen, Direct Antiglobulin Test (DAT), and Indirect Antiglobulin Test (IAT), to detect and identify RBC antibodies.
What is the Western Blot technique used for?
The Western Blot technique is used to identify specific antibodies or antigens in a sample. We utilize this technique to confirm the presence of RBC antibodies.
How do RBC antibodies affect patients with autoimmune hemolytic anemia?
In autoimmune hemolytic anemia, the immune system produces antibodies against the patient’s own red blood cells, leading to their destruction. We provide diagnostic and therapeutic solutions to manage this condition.
Can RBC antibodies cause problems during pregnancy?
Yes, RBC antibodies can cause hemolytic disease of the newborn if the mother’s immune system reacts against the fetus’s red blood cells. We offer guidance on monitoring and managing this condition.
How are transfusion reactions due to RBC antibodies prevented?
We prevent transfusion reactions by performing compatibility testing, including RBC antibody screening, before transfusion to ensure safe blood transfusions.
Leo Bios
Hello, I’m Leo Bios. As an assistant lecturer, I teach cellular and
molecular biology to undergraduates at a regional US Midwest university. I started as a research tech in
a biotech startup over a decade ago, working on molecular diagnostic tools. This practical experience
fuels my teaching and writing, keeping me engaged in biology’s evolution.





Leave a Comment
Your email address will not be published. Required fields are marked *